Growing scientific insight into the gut–brain axis is transforming how diet, digestion, and mental well-being are understood. Once treated as largely independent systems, the gut and the brain are now recognized as deeply interconnected, engaged in continuous two-way communication that influences mood, stress responses, immune function, and cognitive performance. This integrated perspective has gained urgency as mental health conditions and digestive disorders become increasingly common across diverse populations, affecting quality of life and public health systems worldwide.
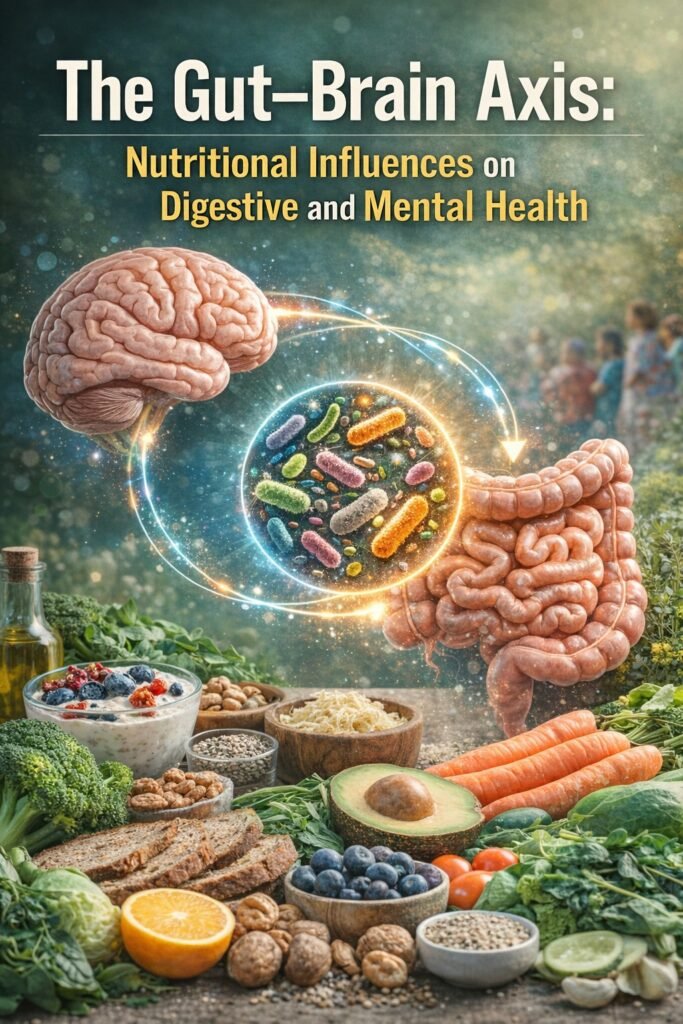
At the center of this connection lies the gut microbiome—a vast and dynamic community of microorganisms residing in the digestive tract. These microbes play a crucial role not only in breaking down food and absorbing nutrients but also in transmitting signals to the brain. Communication occurs through multiple pathways, including neural connections, hormonal signaling, and immune system responses. Because this interaction is bidirectional, psychological stress can disrupt digestion, while imbalances in gut health can influence emotional stability, stress tolerance, and mental clarity.
The gut also serves as a major site for the production of neurotransmitters, the chemical messengers that regulate mood, sleep, motivation, and behavior. A large proportion of these compounds are synthesized or influenced by gut activity, helping explain why digestive discomfort often coexists with anxiety, irritability, low mood, and sleep disturbances. Societies with high consumption of heavily processed foods frequently report elevated rates of both digestive complaints and mood-related symptoms, suggesting that dietary habits play a meaningful role in shaping this relationship.
Modern lifestyles increasingly favor diets rich in refined carbohydrates, added sugars, unhealthy fats, and ultra-processed foods. Such patterns can disrupt the balance of beneficial gut bacteria, promote chronic inflammation, and interfere with normal neurochemical signaling. Over time, these changes may reduce resilience to stress and contribute to both digestive dysfunction and emotional instability. At the same time, ongoing psychological stress and poor sleep can further alter the gut environment, reinforcing a self-perpetuating cycle of physical and mental strain.
Certain groups experience these effects more acutely. Digestive disorders are more frequently reported among women, and individuals experiencing anxiety or depressive symptoms are significantly more likely to suffer from chronic gastrointestinal complaints. In many low- and middle-income countries, rapid urbanization and shifts toward highly processed, Western-style diets have coincided with rising rates of metabolic disorders, digestive problems, and mental health concerns, underscoring that gut–brain health is a global issue rather than one confined to affluent societies.
Nutrition plays a central role in supporting a healthy gut–brain connection. The primary goal is to encourage a diverse and resilient gut microbiome while minimizing inflammation and promoting balanced neurochemical activity. Diets centered on whole, minimally processed foods provide essential fiber, vitamins, and minerals that nourish beneficial bacteria. Adequate dietary fiber supports the production of compounds that protect gut integrity and regulate immune responses. Fermented foods introduce helpful microorganisms that can strengthen digestive function, while healthy fats—particularly those from plant and marine sources—support brain health and reduce inflammatory processes. Consistent hydration and regular meal patterns further aid digestion and help stabilize hormonal signals related to appetite and stress.
Although nutrition alone cannot replace medical or psychological care, improving gut health through dietary choices is increasingly recognized as a valuable complementary strategy. Physical activity, sufficient sleep, mindfulness, and effective stress-management practices further reinforce the gut–brain connection, contributing to overall mental and physical resilience.
As digestive complaints and mental health challenges continue to rise, the gut–brain axis offers a more integrated understanding of human health. Emotional well-being does not exist separately from physical processes, and dietary habits influence far more than digestion alone. A growing body of knowledge points to a clear conclusion: what we eat shapes both our gut environment and our state of mind. Public health approaches that encourage nutritious diets, reduce reliance on ultra-processed foods, and promote balanced lifestyles have the potential to improve digestive and mental health simultaneously, fostering healthier individuals and communities across diverse settings.